
Illustration by Matt Haney, GPJ
KALANGALA, UGANDA — The gentle morning sun casts an orange glow over the beehive of activity on Lake Victoria’s Mwena landing site: oval-shaped commercial boats bringing in catches of Nile perch and tilapia, more than 100 fishermen cleaning and sorting their nets.
Among them is Augustine Kajungu. A fisherman, like his father and grandfather before him. A native of Kalangala, a hard-to-reach district in central Uganda, with a population of 67,200 spread across more than 80 small islands. A father of four. And HIV positive.
“It’s common here,” he says of his HIV status, which he discovered four years ago after seeking treatment for a persistent cough. He has been taking antiretroviral drugs provided free at government health facilities ever since.
Kajungu speculates that he acquired HIV from his relations with sex workers; he declines to disclose his wife’s HIV status, citing the stigma that remains about the condition, despite its high survival rate and his community’s reluctance to exercise caution.
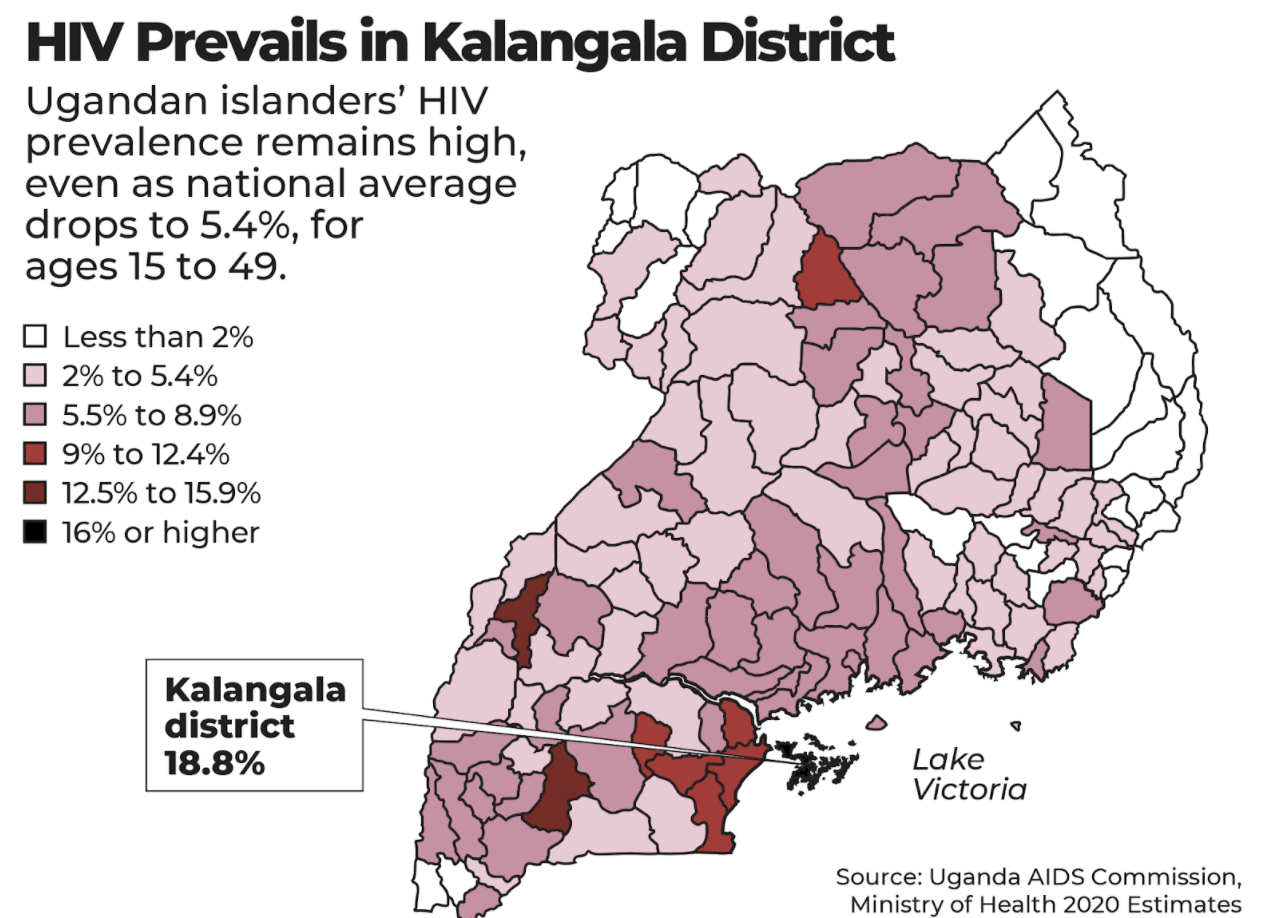
As the rest of Uganda and the world coalesce around reducing HIV infections and increasing access to treatment, Kalangala district is one of the places where geographic and cultural barriers have thwarted these efforts. According to the Uganda AIDS Commission, the district’s HIV prevalence is estimated at 18.8% — more than three times the 5.4% national average — for people ages 15 to 49.
Sub-Saharan Africa’s fishing communities have relatively high HIV prevalence due to their poor health infrastructure, high mobility, transactional sex practices and high alcohol consumption, according to a 2021 research article published by the scientific journal PLOS ONE. In Kalangala, the virus flows freely between the fishermen and the community’s sex workers, a high-risk group fearful of seeking help due to the illegal nature of their work, and with limited funds for boat trips to a clinic.
“Residents there have to make difficult decisions to access treatment,” says Lillian Mworeko, executive director of the International Community of Women Living with HIV in Eastern Africa.
For Ugandans who are willing and able to ask for help, the region’s health agencies offer a range of medications that previous generations would have considered miraculous: drugs taken before sex to prevent acquiring HIV, drugs taken after sex to prevent infection, drugs taken during pregnancy to prevent transmitting the virus to the fetus.
Circumcision for men older than 18 — a practice that may reduce the risk of heterosexually acquired HIV infection by up to 60%, according to World Health Organization analysis — and condom supplies are among the free offerings, says Daniel Byamukama, head of HIV prevention at the Uganda AIDS Commission, a government body that coordinates the country’s HIV prevention efforts.
But Solomon Adoko, a clinical officer at AHF Uganda Cares in Kalangala Health Center IV, one of the largest providers of HIV/AIDS care in Uganda, says the center struggles to reach people on the district’s remote islands to offer counseling, education and medical treatment. Of the 170 patients seen in a typical week, he says, most are fishermen who say they could die from drowning at any time and want to spend their money and enjoy their lives until then.
Byamukama agrees that such fatalistic attitudes make it difficult to convince many fishermen to take care of their health.
“They have a difficult culture that encourages HIV spread,” he says. “They believe that dying from drowning in the lake is more immediate than dying of HIV.”
As for women who would like to seek treatment, Mworeko says, they still need enough money to pay for a boat trip to the nearest clinic.
Harriet Nabanjja, 35, a mother of two, is a sex worker living in Kalangala district who says she learned of her HIV-positive status in 2008. She discloses her status to her customers, she says, but many fishermen still refuse to use protection in their encounters.
“Here fishermen have a lot of money, and they don’t want to use condoms,” she says. “They can give as much as 300,000 [Ugandan] shillings [$85] because they know they will make the money the following day when they go to the lake.”
That’s a significant payment in a country where the median monthly household income for salaried workers is $49, according to 2017 data reported by the Uganda Bureau of Statistics. “Most sex workers are not educated, and they are single mothers,” she says. “They see no value in life and decide to go without condoms.”
Given that Kalangala is accessible only by boat, Byamukama says not many nongovernmental organizations and international agencies are willing to invest the time and money to go there. Both groups they need to reach are also difficult to convince without a long-term commitment.
“We talk to sex workers to demand for condom use for every sexual encounter, but sex workers seem to want money more than their health,” he says. As for the fishermen, “they are a mobile group difficult to track down to offer medical services. You may start him on a service today, and tomorrow they move to a different island.”
One exception is Mohamed Sserwadda. Born and raised in Kalangala district, the 33-year-old finds it alarming that so many of his colleagues have acquired HIV. He has bucked cultural norms by bringing his wife and three children with him from Masaka, a neighboring district, to reduce the temptation to spend his money on sex workers.
He and his wife get tested for HIV several times a year. The tests are free and easy to obtain discreetly, he says, with results available the next day.
“I have dreams. I want to invest for my children,” he says. “When I get HIV, I feel I might become hopeless and not work as hard, so I try to avoid it.”
The community requires a new public education campaign that focuses on the importance of taking precautions to avoid contracting and spreading HIV — without increasing the stigma, says Adoko, the clinical officer.
“There is need to sensitize the local council leaders, opinion leaders, boat owners on landing sites, to change the perspectives of the people.”
Apophia Agiresaasi is a Global Press Journal reporter based in Kampala, Uganda.
TRANSLATION NOTE
Apophia Agiresaasi, GPJ, translated some interviews from Luganda.



